Promoting Patients' Nutritional Health During and After Treatment
Good nutrition is an important component in any patient's cancer journey. A healthy diet is needed to maintain appropriate body weight and strength, absorb the proper nutrients, keep body tissue healthy, and fight infection.
Philippa Cheetham, MD, Jeanne Ann Braddick, MS, RD, CSO, Robin McConnell, MS, RD, CSO, Rebecca Hirsch, MS, RD, Heather Younker, RD, CNSC
Philippa Cheetham, MD, Jeanne Ann Braddick, MS, RD, CSO, Robin McConnell, MS, RD, CSO, Rebecca Hirsch, MS, RD, Heather Younker, RD, CNSC
Good nutrition is an important component in any patient’s cancer journey. A healthy diet is needed to maintain appropriate body weight and strength, absorb the proper nutrients, keep body tissue healthy, and fight infection. Certain types of cancer and treatment, however, can affect nutrition, making eating habits of patients with cancer much different from those for most people.
As defined by the National Cancer Institute, the main goals of nutrition therapy throughout treatment are to replenish missing nutrients, maintain nutritional health, and prevent further problems such as muscle and bone loss.
Four dietitians from the John Thereur Cancer Center (JTCC) at Hackensack University Medical Center sat down recently with Philippa Cheetham, MD, of Winthrop University Hospital, for a Cure Connections roundtable to discuss nutrition during cancer treatment and shared insights on obesity and cancer risk, malnourishment, treatment effects, food, and cooking. Nutritional support at JTCC involves five registered oncology dietitians who offer nutrition counseling to patients and work closely with the patients’ nurses, oncologists, and psychosocial services staff.
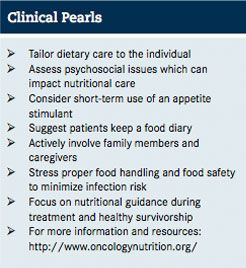
Before a patient begins treatment at JTCC, he or she is screened by the dietitians who ask questions regarding weight changes, changes in food preference, problems affecting eating and physical ability, in order to assess how well the patient’s body can handle the effects of treatment and develop a personalized dietary care plan. Patients receive information about their dietary needs before, during, and after treatment through individual and group counseling. The center also offers nutrition classes in its cooking studio, which opened in 2011.
Risk Factors
Excess body weight, poor nutrition, and physical inactivity are linked to 1 in 3 cancer deaths in the US, according to the American Cancer Society, and excess body weight contributes to as many as 1 in 5 cancer deaths.
Obesity has been associated with an increased risk of gallbladder, esophageal, endometrial, breast, pancreatic, kidney, colon, and thyroid cancers, noted Rebecca Hirsch, MS, RD.
“We do know that with excess body weight, a person’s immune system can be impacted, making them more prone to infection and oxidative damage,” she said. “It can lead to chronic inflammation and the overexpression of certain hormones like insulin and estrogen.”
Hirsch added that insulin has been linked to cancer risk and certain types of breast and endometrial tumors have receptor sites that respond to excess estrogen.
recipe
Some of the patients are referred to JTCC after they’ve already had treatment at another hospital, which poses additional challenges.
Heather Younker, RD, CNSC, pointed out that many of her patients have undergone stem cell transplants and “they are already coming in with deficits of weight and protein losses, muscle mass losses, and nutrient losses.”
The dietary care is tailored to the individual, and Hirsch added that the psychological impact of cancer treatment is an important aspect of nutritional care as well.
“I think when people come to the end of their treatment, they feel that they don’t know what to do,” she said. “They’ve never been at this point, and they’ve experienced side effects which really kind of caused them to not enjoy foods that they traditionally enjoyed for years and years, so they’re snacking on new things because of new cravings and they’re more fatigued … they’re kind of at this standstill, and they’re depressed.”
Treatment Effects
Many types of cancer treatment can change the way patients taste. The shock of suddenly not liking something you’ve always enjoyed eating can be overwhelming, Hirsch explained, which is why nutritional therapy is so important during treatment.
“Patients complain because of the treatment they’re receiving, the changes in taste, their dry mouth, the feeling of constant nausea and probably vomiting, inability to tolerate food really well. They think it’s the food and it might be because of the side effect,” Younker said. And, resistance to eat can result in malnutrition. To help address the changes in taste, these dietitians offer some "tricks of the trade" to patients, including sucking on lemons or lemon drops, rinsing with water and baking soda, using different-flavored toothpaste, or scrubbing the tongue with a toothbrush to stimulate the taste buds.
Weight loss can also be a symptom of the cancer itself, which makes the patient vulnerable to adverse effects of treatment because of nutrient loss and muscle mass loss. Lack of nutrients also prevents healthy tissue from building, puts the patient at risk of infection, and slows recovery time.
“What I find is that cancer patients who are losing weight feel like they’re dying. They feel like their disease has taken over,” said Robin McConnell, MS, RD, CSO. “Sometimes short-term use of an appetite stimulant can really be helpful because if the patient can start eating better, they’ll start to feel better and it also will enable them to be healthy enough to be able to get that next dose of chemo.”
Many patients undergoing hormonal therapies experience weight gain because the treatment slows their metabolism. Patients taking steroids have increased appetite. Hirsch noted that patients need to actively counter such side effects.
“The good news is that it’s poor nutrition and physical inactivity that lead to weight gain,” she said. “It’s up to the patient to stay physically active and just consistently make healthy food choices in an effort to reach any weight goal that they set for themselves.”
She added that she recommends keeping a food diary so that the patient can see on paper how much they’re eating.
“People want to admit only so much,” she said. “But that’s where you come in as an educator and the best thing you can do is put forth information that will inspire them.”
Nutrition Support in Action
The dietitians at JTCC bring their advice to life every week in their onsite cooking studio where they hold cooking demonstrations and classes, offer dishes and samples, and provide cancer-fighting recipes.
Hirsch said that she recommends patients get their protein through lean sources such as chicken, turkey, fish, eggs, nuts, and seeds.
“I think a plant-based diet is the healthiest diet,” she said. “Striving to have at least 2½ cups of raw fruits and vegetables or cooked fruits and vegetables on a regular daily basis is a good way to go.”
Research shows that women need to get 21 to 25 grams of fiber daily, and men need 30 to 38 grams daily depending on age.
McConnell added that they have segments in the studio with patients about alternative sources of calcium, such as soy, rice, almond, and hemp milk.
“We kind of broke down the nutritional pros and cons of each of them, and it gave people an opportunity to try different milks,” McConnell said. “We’re able to have samples of things for patients to try so that they don’t have to spend money on things that they may not like.”
Along with recipes and cooking, the dietitians also teach about proper food handling and food safety.
takeaways
“Especially for the bone marrow transplant population, they have become so immunosuppressed … that they’re susceptible to infections very easily—food-borne illnesses or food poisoning—so that’s when it’s appropriate to teach them how to approach food safety, what foods to be careful of,” Younker said.
And the lessons don’t stop at the cooking studio. The dietitians encourage family members and caregivers to join patients in the classes.
“I think it’s very, very important to get involved with whoever the support system is that a patient may have, whether that person is living in the same home,” said Jeanne Ann Braddick, MS, RD, CSO. “I definitely try to get family members and caregivers involved and find out who’s the one that’s preparing a lot in the kitchen.”
While most of the patients attending classes at JTCC’s cooking studio are actively undergoing therapy, the dietitians stress that good nutrition needs to continue even after treatment ends.
“We do try to focus on diets not only for cancer but also diets that are going to take people into long-term survivorship,” McConnell said. “The diet that we would recommend for healthy survivorship is also going to help somebody prevent heart disease, maintain bone health, and reduce risk of diabetes.”



